Abstract
Mumbai, like any other Metro city, has its own share of contentious issues influencing psychiatric management. These could be old ongoing issues like myths about medications, electroconvulsive therapy and counselling, or newer ones like our stand on homosexuality and crime related to psychosocial factors. A range of these issues is considered in this paper along with some possible solutions. Getting due credit and status for psychiatry as a medical branch is also a challenge we need to address.
Keywords: Bombay Psychiatric Society, Counselling, Electroconvulsive therapy, Homosexuality, Medication, Psychiatry, Quackery, Stigma
Introduction
At the outset, let me thank members of our Society for this honour. It is a huge responsibility, and I will do my best to do justice to this position.
I also take this opportunity to thank all those who have contributed in whatever little I have achieved. First of all I would like to thank my teachers from various psychiatric Units and Departments. I will not name them because the list can never be complete, but each one has contributed something to my growth. I wish to also thank all my patients who added to my knowledge and experience and my family members and friends for their support. And, last but not the least, my late parents for all their encouragement.
I wish to make a special mention of my late father Dr. V. N. Bagadia in whose name we also have a Lifetime Achievement Award in the Bombay Psychiatric Society (BPS). He played a pivotal role in shaping my life, and of many more of his students, some of them sitting here and others in various positions all over the world. In fact, he is the sole reason for me to join psychiatry, and today I am honoured to hold the same position held by him about 40 years back as BPS President. You are all aware, besides all his great achievements, he was one of the founder members who struggled to ensure that the Society did not die a premature death in those early years. The result is there in front of you. With your co-operation and blessings I wish to take it higher.
Mumbai Psychiatry: Current Obstacles
Looking back at 25 years of my association with the field of Psychiatry, there are some very positive developments while some areas have remained either unchanged or have deteriorated. These negative trends, which prevent psychiatry from getting its due status, are the ones that are disturbing me and hence I have decided to bring it to your notice. My vision presently is restricted to Mumbai city because we do not have much say in the National Mental Health plan or policy, either in an individual capacity or of the BPS as a body. Some issues, which I would like to highlight, are common to private practice and full-timers and there are some very specific to the individual set up.
Purely from a clinician’s perspective, ongoing spread of myths and misinformation about our branch is our biggest problem (Singh, 2014[6]). It will not disappear on its own, and we will only have to look for solutions within our framework. Psychiatry and psychiatrists are by-passed by this subtle anti-psychiatry campaign that cannot be ignored. Presently if there is one force working for timely psychiatric intervention, then there are ten forces working against it. Over the years, new ones are getting added to these forces, and it is my feeling of helplessness that drives me to raise my voice and make some noise.
Coming to some very specific disturbing trends.
Misinformation about medication
I am sure all the psychiatrists sitting here have faced this situation wherein patients are told by some Tom, Dick and Harry how psychiatric ‘drugs’ are harmful. But now, in addition, you are likely to have an over-wise chemist also doing the same damage. Some of them till yesterday were running a grocery shop and have now acquired a licence for a chemist’s shop doing home delivery of medicines. Such unqualified chemists are a perfect source of misinformation. A barely motivated patient easily gets demotivated because of the piquant situation that the businessmen himself is condemning the goods he is supposed to sell. The next-door chemist is the busiest primary care physician, and some psycho-education should be designed for them to reduce this damage.*
Electroconvulsive therapy
Misinformation about electroconvulsive therapy (ECT) is shocking, and we are ourselves becoming more and more defensive thanks to the entire stigma associated and the hurdles we face in the execution of electroconvulsive therapy in the private set-up. This is an unfortunate development because unknowingly we have pushed a life-saving remedy into a reserve category. In spite of the fact that the number of ECTs has gone down significantly, at least in the private set up, the taboo linked with ECT and the psychiatrist remains. Probably, there is also the need to find out some other mechanism to induce a convulsion so that the word ‘electro’ and ‘shock’ can be dropped.
Quackery
Our cultural and spiritual heritage is exploited in a vulnerable population. It could be a tantrik operating from some dargah or hotel room, one who can freely advertise wherever he wants including in local train compartments. It could also be a guru or a religious faith-healer operating through some cable channel network. One who can also oversell yoga or herbal remedies and tell you to stop medication. Over and above this, patients are bluntly told that a doctor cannot understand these spiritual and divine mechanisms. Psychiatric patients and their relatives are the most vulnerable targets of such practices.
Are these things going to stop on their own? It is difficult to talk against spirituality or religion in this country, but we all know how these issues are exploited. Should we not raise a collective voice against it?
Counselling
The word ‘Counselling’ has really become a selling point and a media driven commodity. This is at the cost of Holistic Psychiatry where each treatment modality has its own significance. I myself believe that no treatment would be complete unless all three that is, bio-psycho-social angles (Engel, 1997[1]) are attended to; but when the word ‘Counselling ‘is projected as a blanket therapy irrespective of its utility in a given case, it adds to much avoidable delay in treating a genuine major psychiatric disorder. Unfortunately, not all the so-called counsellors are adequately qualified. You can open a shop with 3-6 months of a certificate course, and there is no regulatory body to control it. I wish our senior colleagues from the field of counselling could do something about it.
Recently, one of the dailies reported how a case of paranoid schizophrenia was controlled after 10 sessions of counselling. In my own experience after 45 min of a psychotherapeutic session a family member asked, ‘Dr. Inka counselling karvaye to kaisa?’** This is when you know that market forces have successfully targeted a vulnerable individual and created a brand name. I would, therefore, urge my fellow colleagues to use the word “counselling” judiciously and not shy away from emphasising the role of biological therapies wherever the credit is due.
Role of other medical branches
The unfortunate part of undergraduate psychiatric training here is the limited exposure that a student has in the form of a ‘Minor’ clinical term of 15-30 days and that too after a student is already bombarded with the somatic side of medical studies. Next opportunity to learn for this doctor is from the medical representatives when they sell psychiatric products to non-psychiatric experts who are willing to use it. So they include a micro dose of a psychotropic drug to their usual prescription when actually what they are handling unwittingly is a pure major psychiatric disorder. I think old time Hindi cinema villain Ajit must be giving command hallucinations: ‘Doctor, tu ise itna hi dose de, taki na woh chain se ji sake, aur na hi woh asani se mar sake!’***
My request to fellow colleague is that during your talks or presentations, do not promote medicines that your non-psychiatric colleague cannot handle. Now with so many non-addicting hypnotics available they should stop using alprazolam or any such benzodiazepine as a ‘Neend ki goli’****. We will have to be proactive in changing this habit.
Overlapping specialities
Psychiatry itself overlaps with other branches, but that is only when behaviour comes into the picture. Now you have specialities of other branches adding to the confusion. Earlier, the patient had to differentiate between only a psychiatrist and a neurologist. Now just like a Child Psychiatrist you have a ‘Developmental Paediatrician’ and ‘Paediatric Neurologist’. At this rate, you will soon have a ‘Behavioural Neurologist’, and why not, we already have Neuro-Psychiatry as a branch. My only concern is that it should not add to the delay in imparting timely care just because now there is another excuse available to avoid seeing a psychiatrist. Sexology is one more such branch that is trying to dissociate, in spite of the fact that whatever training most doctors have in sexology is imparted by psychiatry departments.
This would mean that we will have to focus now on helping patients understand these differences and I suppose we should not hesitate in doing so.
Other areas adding to treatment delay
Lack of insurance coverage (Mediclaim 2012 Policy Document[3])
Simple economics teaches you that when you are paying a premium you should also know how to make a recovery. A psychiatry patient with Mediclaim gets admitted under some other specialist with some vague diagnosis and the due credit that should come to psychiatry is lost.
Psychiatry in corporate or private hospitals
Barring a few, psychiatry in most 5-star hospitals is reduced to Consultation-Liaison Psychiatry. Most of them do not allow indoor care for psychiatric patients. Thus, middle and upper class population’s exposure to psychiatry becomes limited, and recognition of the branch is compromised.
Licensing for psychiatric nursing home
This has deprived a large chunk of the middle class from necessary treatment, e.g., short-term hospitalisation. They can neither go to government or municipal hospitals nor can they afford the licensed set-up. Here, legislation has affected growth of the branch. A bitter pill we had to swallow.
Association Should Play a Proactive Role
So why am I cribbing about these issues? At least some of them can be addressed if the Association decides to play a proactive role because nobody is going to fight the battle on our behalf. We will also have to remember that thanks to the massive efflux of our trained psychiatrists to foreign lands, our number is still negligible compared to the population we are dealing with. The need to be proactive on this and related issues is not out of insecurity but to avoid complacency that is very common in a busy metro life. Unattended contentious issues often take non-scientific routes adding to the myths and misinformation about the field. Proactive approach is likely to help us fight stigma attached to the branch.
Some More Complex Issues Staring us in the Face
As I envisage, there are some more complex issues that are staring at us in Mumbai, and a time will come when either we will have to take a stand or somebody else will take a stand that we may not find palatable. Some of these issues are:
Unhealthy and unchecked rise in alcohol (Telegraph, 2011[7]) and cannabis consumption.
Criminal activities linked with personality factors and its handling by police and judiciary.
Our stand on Homosexuality as per Section 377 of IPC[5] (Delhi High Court, 2009[2]).*****
School mental health, controversies of Right to Education (MHRD. Right to education, 2009[4]), Quantification of Learning Disability are some of the newer challenges. Take, for example, Autism. I am sceptical about the kind of statistics that are being quoted in the media. It is very easy to jump on a bandwagon when media and celebrities get involved. (A celebrity endorsed event quoted incidence of autism at around 1 in 110 children).
Our handling of the media – now that they need us and we need them.
Role of alternative therapies – Are they going to complicate the management of a psychiatric patient or have some complementary or supplementary role? As such there is no mechanism for easy crossover, and if things do not work out there is only one obvious scapegoat, that is, psychiatric medicines.
Role of Bombay Psychiatric Society
That brings us to the role of the BPS in the current scenario. We will have to get involved in areas other than academics and do something much more to undo the faulty image that is thrust upon us. My contention is that as an Association we should raise our collective voice on all these and other contentious issues.
Conclusions [Figure 1: Flowchart of paper]
Figure 1.
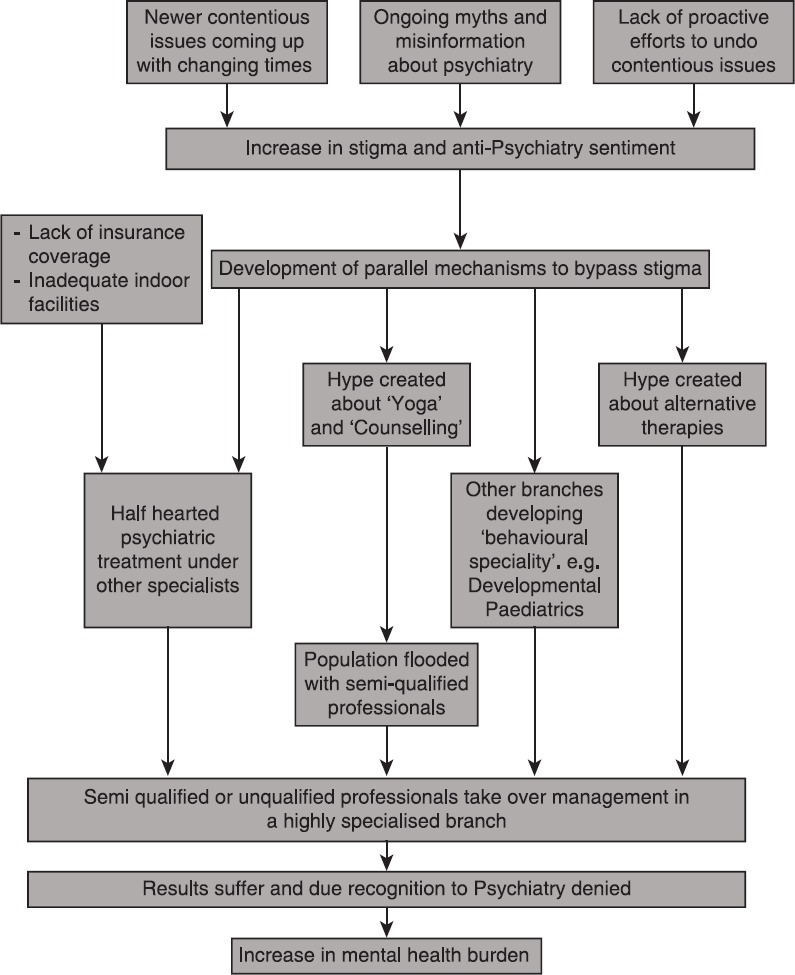
Flowchart of paper
Psychiatry in Mumbai has gone through a lot of ups and downs in the last 25 years. It is important not to ignore the downs. Misinformation about old issues like medication, ECT and quackery have persisted and, if at all, increased. New issues like unqualified ‘counsellors’ and hurdles in hospitalisation of psychiatric patients are getting added. In future, we can anticipate conflicts on some issues like homosexuality, criminal justice or school mental health.
If we are not able to resolve all such developments effectively, they will add to the stigma linked with the branch. Identification of and addressing such contentious issues on a continuous basis are a necessity for our Association.
Take Home Message
Contentious issues including those specific to Mumbai should be addressed without complacency for the growth and recognition of Psychiatry as a stigma free medical branch.
Questions that this Paper Raises
Should geography specific issues of a speciality be dealt with by individuals or by an Association of professionals?
Are Psychiatrists in metro cities like Mumbai too busy to address conflicts in imparting basic mental health services?
About the Author

Sanjay Bagadia MD received his under-graduate and post-graduate (Psychiatric) training at Seth G. S. Medical College and K.E.M. Hospital, Mumbai, India. Apart from private practice he is attached to Mahavir Medical and Research Centre, Khar, Mumbai, India. Formerly he was a Part time psychiatrist with Bombay Hospital, Marine Lines, Mumbai and Honorary Psychiatrist with Lion Tarachandbapa hospital, Sion, Mumbai.
Acknowledgment
Grateful thanks are due to all my patients who enriched my understanding of Psychiatry. My debt of gratitude is also due to all my teachers, and to my father Dr. V. N. Bagadia, for imparting me the basic vision to appreciate the subject of Psychiatry.
*This speech was delivered before the Indian Food and Drug Administration struck down on unqualified chemists.
**Translated to mean: ‘Doctor, what about counselling for this patient?’
***Translated to mean: ‘Doctor, you give him just as much of a dose as he cannot live comfortably with, and also as much as he cannot die in ease with!’.
****Translated to mean, ‘Sleeping tablet’.
*****In Dec-2013The Supreme Court of India overturned the Delhi High Court judgement of 2009.
Conflict of interest
None declared.
Declaration
This is my original unpublished piece, not submitted for publication elsewhere.
CITATION: Bagadia SV. Mumbai psychiatry: Current obstacles. Mens Sana Monogr 2015;13:171-179.
Peer reviewer for this paper: Anon
References
- 1.Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129–36. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 2.Delhi High Court. Naz Foundation versus Govt. Of NCT of Delhi and Others; Judgement Dated; July 2. 2009. [Last accessed on 2015 Feb 13]. WP[c] No.7455/2001. Available from: http://www.indiankanoon.org/doc/100472805 .
- 3.Mediclaim 2012 Policy Document. What are excluded under this Policy; 4.4.6.1. UIN: IRDA/NL-HLT/NIA/P-H/V.I/330/13-14. IRDA, GOI. [Last accessed on 2015 Feb 13]. Available from: http://www.newindia.co.in/downloads/Mediclaim-2012-Policy-Document.pdf .
- 4.MHRD. Right to education. RTE Act and Article 21-A Right of Children to free and compulsory education Act-2009, Ministry of HRD-GOI. [Last accessed on 2015 Feb 13]. Available from: http://www.mhrd.gov.in/rte .
- 5.Section 377 of IPC. Unnatural offences. Central Govt Act. [Last accessed on 2015 Feb 13]. Available from: http://www.indiankanoon.org/doc/1836974 .
- 6.Singh AR. The task before psychiatry today redux: STSPIR. Mens Sana Monogr. 2014;12:35–70. doi: 10.4103/0973-1229.130295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Telegraph. Mumbai votes to increase alcohol age limit. 2011. Jun 2, [Last accessed on 2015 Feb 13]. Available from: http://www.telegraph.co.uk/news/worldnews/asia/india/8552279/Mumbai-votes-toincrease-alcohol-age-limit.html .

