Abstract
This paper talks of support systems for mental health professionals wherein the Bombay Psychiatric Society (BPS) should devote some meetings exclusively to problems pertaining to the profession, e.g., long and odd working hours leading to potentially hazardous practice schedules, unhealthy competitive attitudes and culture. A crash course in self-defence against potentially psychotic patients and drug addicts is advocated as also awareness of the potential hazards in dealing with the litigious paranoid patients, erotomaniacs and some of the difficult hysterical patients. Potential medicolegal problems arise in treating an uncooperative patient without his knowledge and consent on an outpatient department basis, admitting such an uncooperative patient to a nursing home or a hospital, administering electroconvulsive therapies, maintaining detailed clinical records of patients, and legal issues involving smaller psychiatric private nursing homes. This paper stresses on the use of Yoga as a recognised psycho-physiological therapy. Furthermore, it suggests on the need for BPS, as a professional body, to have a cell to guide and help aspiring young professionals in setting up private practice. It points out the need to evolve some concrete programmes that in the long run should help alleviate stresses and strains and promote positive comprehensive health amongst mental health professionals.
Keywords: Medicolegal problems, Private practice, Support systems for mental health professionals, Yoga
Introduction
I have been associated with the Bombay Psychiatric Society (BPS) for the last 20 years and feel greatly honoured to be its President. All the same, I feel humble when I think of the great stalwarts who have earlier served as Presidents of the Society. Amongst this galaxy of luminaries are my senior teachers, mentors, colleagues and friends. I am thankful to all these predecessors, who have been instrumental in the healthy growth of our Society over past several years. They have made our task much easier.
Standing on their shoulders, so to say, I am sure, with your cooperation, good wishes, expert guidance and active participation, I will be able to carry out my current responsibility to the Society. I have served the Society in the capacity of an Executive Committee Member and Honorary Secretary in the past and with the blessings of you all, am assuming the mantle of Presidentship today.
Support Systems for Mental Health Professionals
I am not much into teaching or research. I am essentially a clinician and hence take this opportunity to try to talk to you about something that is of practical importance. It has been my mind for the last couple of years.
In the past 2 years, we witnessed the sad and untimely demise of two of our professional colleagues by way of suicide. It is a known fact that amongst all medical professionals, psychiatrists and anaesthetists are maximally prone for suicide and drug abuse. Psychiatric profession is highly taxing emotionally. On one hand, ours is one of the most unglamorous of medical specialities. We are considered and treated as a stepchild of medicine. It is also relatively much less remunerative as compared to most other branches of medicine. On the other hand, professional risks have increased many folds in the last few years, thanks mainly to the consumer protection act.
Many of you must still remember that unfortunate incident which occurred last year, in which one of our respected senior colleagues was framed in one of the weirdest, most illogical and irrational of medicolegal cases. One can imagine how much embarrassment, mental agony and torture it must have caused the concerned colleague of ours; and the bitter fact is that we, as an organised body, have not done much beyond offering lip sympathy in such cases.
Such cases only underline the fact that, we, as mental health professionals, are extremely vulnerable to various stresses and strains arising out of our professional practice, leading to frustrations and depressions. When our own mental stability, mental soundness, our sanity is at risk, I wonder how we can project ourselves as moulders and healers of the society at large.
Being concerned about our patient’s well-being is undoubtedly our prime duty, but in doing or overdoing so, we need not neglect our own selves. I sincerely feel that we have not thought seriously about the betterment of our own fraternity. It is high time that we first set our own house right, only to be more effective and efficient in taking care of our patients.
In view of this, I have decided to touch upon some of the aspects of the hitherto most neglected area, that is, support systems for the mental health professionals. Although it is not a new concept, there is hardly any literature available on this topic even in the Western Textbooks of Psychiatry. I even tried to look for references in the American and British Journals of Psychiatry and psychotherapies, but unfortunately drew a blank. This only goes to show that even in the West, it is a somewhat neglected area. Under the circumstances, whatever I am going to speak today is my own thoughts and observations. You could call it thinking aloud.
At lot has been written and is being practised for helping the various types of patients’ groups and even for their relations, but self-help group for Mental Health Professionals is not very common. Nobody seems to be thinking seriously about their problems. Of course, there are certain basic things that are being observed and practised as regards the well-being of mental health professionals in the USA and also in the UK. There, it is mandatory for all mental health professionals to see another professional consultant colleague periodically – say once a fortnight or once a month – to verify and check their own mental stability. Furthermore, it is quite a common practice there to hold regular periodic meetings of a group of professionals, wherein consultants as well as post-graduate students are not only expected to, but also in fact encouraged to give vent to the negative feelings they experience in the course of their interaction with patients. At such meetings, not only therapeutic dilemmas are discussed and debated, and concrete guidance offered by senior professional colleagues, but also personal issues bothering individual students or professionals are dealt with and practical advice is offered.
In our monthly clinical meetings, wherein we mainly deal with diagnostic dilemmas, present unusual cases and overview of literature pertaining to such cases and topics, if we could incorporate the aspects mentioned earlier, or if we could devote some meetings exclusively to the problems pertaining to our profession in general and professional colleagues in particular, it would help many of us a great deal, particularly those who are not attached to major teaching hospitals and as a result find it difficult to have professional interaction with a larger group of fellow professionals. Such a practice would certainly reduce the sense of alienation that usually creeps into the professionals who are not in the mainstream.
Issues like longer and odd working hours, leading to potentially hazardous practice schedules, unhealthy competitive attitudes and culture are some of the areas where we could have deliberations amongst ourselves. Following analytical model in this regard – forming smaller and more cohesive groups of consultants in the different prominent pockets of this metropolis and holding regular meetings of such groups would also be helpful. Evolving recreational activities and facilitating periodic vacations for individual professional members by rotation are some of the things that are being practised in smaller cities and towns even in India. We could easily follow this practice in our city by way of forming smaller local groups. This would lead to more cohesive and cooperative functioning rather than competitive functioning.
This is very important particularly in the Indian context as ours is essentially an isolationist pattern of practice unlike the West where group practice is prevalent and, as a result, the entire group shares the whole burden of practice.
In the United Kingdom, all prospective post-graduates, before starting their residency programme, are given a crash course in self-defence against potentially psychotic patients and drug addicts. How to tackle assaultive patients and how to physically protect oneself from them is taught to them systematically as part of their post-graduate curriculum. Although socio-cultural conditions are quite different here from that in the western world, and physical assault on a mental health professional by a psychotic patient is not a very common occurrence, offering such a systematic training to our young budding professionals is not a bad idea. On similar lines, if potential hazards in dealing with the litigious paranoid patients, erotomaniacs and some of the difficult hysterical patients could be highlighted and practical tips offered as to how to get rid of them, it would be quite helpful to the inexperienced, raw postgraduates.
Psychometric Screening of Post-graduate Students
It would be worthwhile to psychometrically screen all post-graduate students right at the beginning of their residency posts. Psychoanalysts have this practice of analysing aspiring analysts before certifying them as qualified analysts. If senior teachers at the teaching institutes get to know the personality profile of their post-graduate students at the outset, they will have three good years at their disposal to work on the individual weaknesses of such students. As per the existing rules of post-graduate admissions, we may not be in a position to prevent someone from taking up psychiatry on the basis of even grossly abnormal personality profile, but we will at least be aware of the pathology and will be able to guide individual students in overcoming it. Orienting them, giving them insight as regards their shortcomings and allowing them to work over their deficiencies under the expert supervision and guidance of senior teachers for three long years will go a long way in making them better adjusted individuals and professionals.
I think Dr. Doongaji used to screen his students on these lines; Late Dr. S. M. Lulla would personally interview post-graduate aspirants at length at the beginning of their training. Similarly, in Nair Hospital, for the last many years, the 1st MBBS students are screened and those having gross problems are followed up subsequently throughout their MBBS course.
I believe, implementing such a practice as a routine at the post-graduate level will help our young psychiatrists to a great deal.
Yoga
Exposure to the indigenous discipline like yoga at this juncture should also be helpful. In the recent past, there has been a lot of research on the use of many eastern techniques of healing in health sciences. A lot of emphasis is being laid on lifestyle and health. Modern era and its increasing stresses call for stress management techniques. Yoga as a recognised psychophysiological therapy offers such techniques in the most effective way. Yoga is not restricted to just body postures, pranayam and meditation. Yoga is a way of life. Positive changes in the personality are brought about most effectively by way of changes in the attitudes of an individual through the 8-fold path of Yoga, i.e., ashtanga-yoga.
Fortunately for us, we have two excellent yoga institutions in our metropolis that have been pioneers in the field, namely the Yoga Institute at Santacruz and the Kaivalyadham at Charni Road.
I strongly believe that yoga has a major role to play in preventing and treating neurotic disorders, personality disorders, psychosomatic disorders, sleep disorders, drug abuse and alcoholism. Its preventive and therapeutic role in these disorders has been acknowledged even in the western textbooks of psychiatry and internal medicine. Furthermore, it has been accepted as an effective type of physiological therapy.
Preventive and Social Medicine Department of KEM Hospital and G. S. Medical College has incorporated visits to Yoga Institute, Santacruz, in its programme for the interns. If we could influence and encourage our post-graduates to adequately expose themselves to this ancient Indian discipline, it would certainly go a long way in helping them become better equipped for treating various neurotic patients as well as for maintaining their own mental equilibrium.
Setting Up Private Practice
One of the biggest dilemmas for any fresh post-graduate is where and how to start private consulting practice. This is one area, which has not been discussed in any of the textbooks nor discussed by senior teachers with the seriousness it deserves. The only honourable exception being Dr. Alan De Sousa textbook of psychiatry, where he has devoted a full chapter to this important but hitherto neglected area (See also pgs 3-15 of this issue).
Sometime back, I had an opportunity to have interaction with one Dr. Shivkumar Hatti, a past student of KEM Hospital, who has been in Philadelphia, USA for last 25 years. He is a consultant psychiatrist and has been involved with the management of professional practice with the help of insurance companies. If we, as a professional body, could have a cell on similar lines to guide and help aspiring young professionals as regards setting up private practice, it will certainly help reduce their hardships in their initial period of uncertainty.
Private Practice
Private practice is altogether a different ball game. It will not be an exaggerated statement if we say that most of the things that we do in private practice today are almost totally illegal. There is a vast difference between what we learn during our post-graduate training days and what we practice as clinicians. There are lot of practical limitations is private practice as a result of which, we are sort of forced to make a lot of compromises. And all this is done in the best interest of the patient.
What criteria, guidelines and situations are preached as ideals in Western textbooks are often not met with in private practice. Unlike most of the other medical conditions where the diagnosis is substantiated by biochemical and/or radiological investigations, ours is essentially a clinical branch which keeps changing depending upon the change in clinical picture over a period of time. In general, we need to go by our clinical acumen, which may not stand in a court of law in the event of medicolegal suits. I think we, as an organised body, should do something concrete to reduce this tension and perpetual sense of insecurity.
Potential Medicolegal Problems
There are certain areas and situations in which we find ourselves most vulnerable and maximally exposed to the risk of potential medicolegal problems. To name a few, they are as follows:
Treating an uncooperative patient without his knowledge and consent on outpatient department (OPD) basis.
- These are usually psychotics, schizophrenics, paranoids, alcoholics or drug abusers.
- This is usually done at the earnest request of patient’s near relation, that is, either a spouse or parent or sibling. It is done in the best interest of the patient.
Admitting such an uncooperative patient to a nursing home or a hospital in a similar situation having the same consideration mentioned earlier.
Administering electroconvulsive therapies (ECTs)
- Informed consent of the patient and relations explaining the risks.
- Criteria for giving ECTs (indications).
- Fulfilling the prerequisites in the form of medical examinations, investigations, anaesthesia fitness, etc.
Lack of definite, practical guidelines or criteria for the use of newer atypical antipsychotics like clozapine.
Maintaining detailed clinical records of our patients and the ethical issues involved therein.
Legal issues involving smaller psychiatric private nursing homes.
If each of these issues could be taken up by a panel of senior, experienced consultant members of our Association and something like a white paper could be published under the aegis of the BPS, giving certain definite practical criteria or guidelines, which would be adhered to by all of us, it would definitely help us develop an additional buffer against potential medico-legal cases. In Poona, I suppose, a similar attempt was made by a group of some 22 psychiatrists some time back. They prepared a questionnaire pertaining to controversial issues for the practicing psychiatrists to fill up and to come out with certain guidelines by way of a consensus.
In the USA, the APA had laid down definite guidelines for various therapies, after taking into account the recommendations received from a panel of psychiatric professionals. On such panels, they have had a judicious mix of research workers and clinical practitioners. We could adopt a similar model in forming guidelines. Ours is a cohesive group of private practitioners as far as the quality and pattern of practice is concerned. Since all of us are practicing in a similar urban set-up, it would not be very difficult to come out with such definite guidelines.
The courts would definitely give more weightage to such white papers, brought out by our professional body by way of consensus, than the expert testimony in individual cases, which is usually considered a biased opinion in favour of a fellow consultant by the judges, in the event of medicolegal cases.
To achieve this and to sort out other medicolegal issues, more interaction with legal professionals is desirable and required. Medical Consultants Association of India has been doing a lot of good work in this regard, but because of the diversities of various specialities of medicine, peculiar/specific problems pertaining to our specialty are not being addressed that effectively. Indemnity for psychiatric professionals, insurance coverage for various psychiatric conditions are some of the issues which could be taken up with legal experts (See also pgs 83-91, this issue).
New Programmes
During the last few years, our Society has grown from strength to strength in its membership. It has developed a well-planned programme of the year’s activities and has a reasonably sound financial base. According to me, this, therefore, is the right time to incorporate some new programmes concerning ourselves into the year’s other regular activities. No outsider is going to do it for us. We will have to take the initiative in this regard and try to evolve some concrete programmes that in the long run should help us all alleviate our stresses and strains and promote positive comprehensive health amongst us.
There is nothing wrong in thinking on these (selfish) lines. I will wind up my Address by quoting Oscar Wilde, who says,
It is not selfish to think of oneself. A man who does not think of himself does not think at all.
Concluding Remarks [Figure 1: Flowchart of the Paper]
Figure 1.
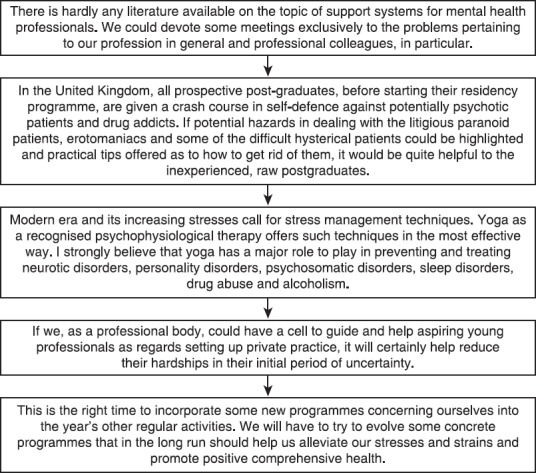
Flowchart of the paper
There is hardly any literature available on the topic of support systems for mental health professionals. It is mandatory at some places for all mental health professionals to see another professional consultant colleague periodically–say once a fortnight or once a month-to verify and check their own mental stability. We could devote some meetings exclusively to the problems pertaining to our profession in general and professional colleagues, in particular. Issues like longer and odd working hours, leading to potentially hazardous practice schedules, unhealthy competitive attitudes and culture are some of the areas where we could have deliberations amongst ourselves.
In the United Kingdom, all prospective post-graduates, before starting their residency programme, are given a crash course in self-defence against potentially psychotic patients and drug addicts. If potential hazards in dealing with the litigious paranoid patients, erotomaniacs and some of the difficult hysterical patients could be highlighted and practical tips offered as to how to get rid of them, it would be quite helpful to the inexperienced, raw postgraduates.
Psychoanalysts have this practice of analysing aspiring analysts before certifying them as qualified analysts. If senior teachers at the teaching institutes get to know the personality profile of their post-graduate students at the outset, they will have three good years at their disposal to work on the individual weaknesses of such students.
In the recent past, there has been a lot of research on the use of many eastern techniques of healing in health sciences. A lot of emphasis is being laid on lifestyle and health. Modern era and its increasing stresses call for stress management techniques. Yoga as a recognised psychophysiological therapy offers such techniques in the most effective way. Yoga is not restricted to just body postures, pranayam and meditation. Yoga is a way of life. Positive changes in the personality are brought about most effectively by way of changes in the attitudes of an individual through the 8-fold path of Yoga, that is, ashtanga-yoga. I strongly believe that yoga has a major role to play in preventing and treating neurotic disorders, personality disorders, psychosomatic disorders, sleep disorders, drug abuse and alcoholism. Its preventive and therapeutic role in these disorders has been acknowledged even in the western textbooks of psychiatry and internal medicine.
If we, as a professional body, could have a cell to guide and help aspiring young professionals as regards setting up private practice, it will certainly help reduce their hardships in their initial period of uncertainty. There is a vast difference between what we learn during our post-graduate training days and what we practice as clinicians. There are lot of practical limitations in private practice as a result of which, one is forced to make compromises. And all this is done in the best interest of the patient.
Potential medicolegal problems arise while treating an uncooperative patient without his knowledge and consent on OPD basis, admitting such an uncooperative patient to a nursing home or a hospital, administering ECTs, maintaining detailed clinical records of our patients, and the Legal issues involving smaller psychiatric private nursing homes
In the USA, the APA had laid down definite guidelines for various therapies, after taking into account the recommendations received from a panel of psychiatric professionals. On such panels, they have a judicious mix of research workers and clinical practitioners. We could adopt a similar model in forming guidelines.
This, therefore, is the right time to incorporate some new programmes concerning ourselves into the year’s other regular activities. We will have to try to evolve some concrete programmes that in the long run should help us alleviate our stresses and strains and promote positive comprehensive health amongst us.
Take Home Message
There is the need to evolve a support system for mental health professionals. BPS, as a professional body, can evolve guidelines for setting up private practice and for various therapies. Awareness of potential medicolegal problems peculiar to psychiatry is a must.
Questions that this Paper Raises
What sort of support system for mental health professionals works best?
What are the does and dont’s of setting up private practice?
How can yoga become an integral part of medical practice?
What medicolegal issues are of paramount importance in psychiatric practice?
About the Author

Ajit Dandekar MD, DPM is a psychiatrist in private practice in Mumbai, India. He was President of the Bombay Psychiatric Society in 1999-2000. He is attached to the Holy Family Hospital, Nanavati Hospital and Jeevan Vikas Kendra, Mumbai. His areas of special interest are Depression, Psychosomatic disorders and psychotherapy.
Footnotes
Conflict of interest
None declared.
Declaration
This is my original unpublished piece, not submitted for publication elsewhere.
CITATION: Dandekar A. Support system for mental health professionals. Mens Sana Monogr 2015;13:114-124.
Peer reviewers for this paper: Anon

